Ghana is facing a growing mental health emergency that demands immediate national attention, strategic investment, and compassionate reform. Deeply rooted spiritual beliefs, severe shortages in clinical services, and widespread stigma are driving thousands of families to seek help in forest prayer camps and faith-based compounds rather than hospitals. This pattern is producing preventable suffering, human rights violations, and tragic outcomes that undermine public health and social stability.
Across urban and rural communities, families describe mental distress in spiritual terms—possession, curses, or witchcraft—and often pursue religious interventions before or instead of medical treatment. Faith leaders and prayer camps are widely trusted and sometimes seen as the only available option when clinical care is inaccessible or perceived to have failed. One faith leader told reporters, “What the doctors cannot cure, God can,” reflecting a belief that spiritual healing is the solution when medicine appears insufficient.
The clinical capacity gap in Ghana is stark. The Mental Health Authority reports just over 80 psychiatrists for a population exceeding 35 million people, leaving most regions without reliable access to specialist care. The authority also estimates that more than one in five Ghanaians—over 21 percent—live with mild to severe mental disorders, while the national health budget allocates only about two percent to mental healthcare. These figures expose a mismatch between need and resources that fuels reliance on nonclinical care and delays evidence-based treatment.
Prayer camps and faith-based centres often operate in cramped, poorly ventilated spaces where patients may be malnourished, restrained, or isolated. Despite a 2017 legal ban on shackling people with psychosocial disabilities, the practice persists in hidden forms; human rights organizations documented chained patients and helped secure releases in recent years. Forced fasting, chaining, and prolonged isolation can worsen psychiatric conditions, increase trauma, and in some cases lead to death, underscoring the urgent need for humane, rights-respecting alternatives and stronger enforcement of existing laws.
Stigma remains a powerful barrier to care. Surveys show that a majority of Ghanaians attribute mental illness to supernatural causes, which discourages help-seeking at medical facilities and reinforces secrecy and shame. When families fear social exclusion or distrust hospitals, they are more likely to turn to spiritual healers who promise immediate miracles and who are embedded in community life. This dynamic perpetuates cycles of neglect and prevents early intervention that could reduce long-term disability and social costs.
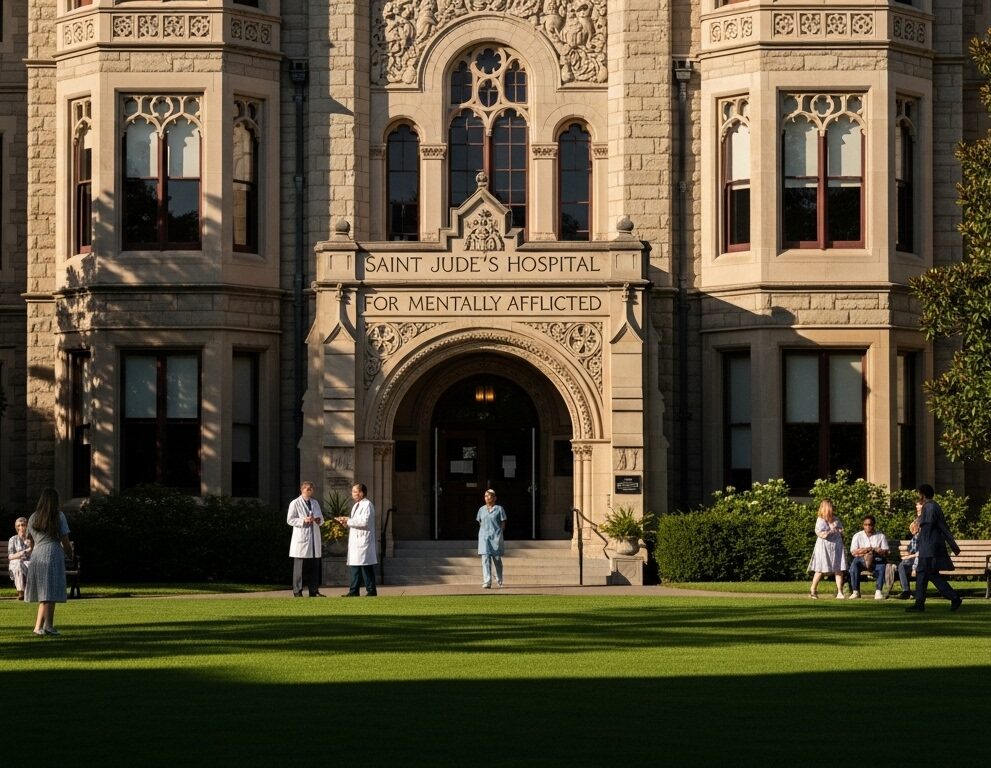
Public hospitals and specialist centres like Korle Bu Teaching Hospital provide critical clinical expertise, but they are overwhelmed and concentrated in major cities. Community-level mental health services are thin or nonexistent in many districts, leaving primary care workers undertrained and families without local referral pathways. Strengthening primary care, training general practitioners and nurses in mental health screening and basic interventions, and expanding telepsychiatry could help bridge gaps while specialist capacity is scaled up.

A pragmatic, culturally sensitive response must engage faith leaders and traditional healers as partners rather than adversaries. Successful public health strategies in other domains have integrated trusted community actors—such as traditional birth attendants—into referral networks and training programs. Equipping spiritual leaders with basic mental health literacy, danger-sign recognition, and clear referral protocols can reduce harmful practices and channel people toward timely clinical care when needed.
Policy reform and budgetary commitment are essential. Increasing the mental health allocation within the national health budget, investing in community-based services, and expanding psychiatric training programs will create sustainable capacity. Legal enforcement against inhumane treatment must be paired with social supports for families, including counseling, respite care, and financial assistance, so that humane options are realistic and accessible for those who now rely on prayer camps out of necessity.
Human rights groups and mental health advocates emphasize that change must be rights-centered. Rehabilitation, psychosocial support, and reintegration services are critical for people who have experienced chaining, abuse, or prolonged institutionalization. Public campaigns that combine factual information with culturally resonant messaging can reduce stigma and encourage early help-seeking, while legal protections and monitoring mechanisms can deter abuse and ensure accountability.
International agencies and global health partners can support Ghana’s response through technical assistance, funding for workforce development, and evidence-based program models. The World Health Organization has documented rising rates of depression and anxiety across Africa since the Covid-19 pandemic, highlighting the need for coordinated regional action and resource mobilization to prevent a widening mental health crisis.
Practical steps that can be implemented now include targeted training for faith leaders on danger signs and referral pathways; mobile mental health clinics to reach underserved districts; public education campaigns that normalize mental health care; and rapid expansion of psychosocial support services for survivors of abuse. These measures, combined with longer-term investments in workforce and infrastructure, can reduce reliance on harmful practices and save lives.

The human cost of inaction is high: untreated mental illness undermines families, reduces economic productivity, and increases vulnerability to abuse and exploitation. Ghana’s cultural strengths—strong community networks and deep faith—can be harnessed to create a hybrid model of care that respects spiritual beliefs while ensuring access to evidence-based treatment and human rights protections. This balanced approach offers the best chance to transform prayer camps from places of last resort into entry points for safe, effective care.
Ghana stands at a crossroads: continue with the status quo, where spiritual remedies substitute for scarce clinical services and human rights violations persist, or commit to a comprehensive, well-funded mental health strategy that integrates community trust, clinical expertise, and legal safeguards. The choice will determine whether thousands more are needlessly harmed or whether Ghana can build a humane, effective mental health system that reaches every region and protects every person in need.
Source: Ghana’s mentally ill trapped between prayer and care