From 1 January to 31 August 2025 a global cholera upsurge produced 462,890 reported cases and 5,869 deaths across 32 countries in five World Health Organization (WHO) regions, with the Eastern Mediterranean Region reporting the largest share of cases followed by the African and South-East Asia regions. During August 2025 alone (epidemiological weeks 32–35), 57,215 new cholera and acute watery diarrhoea cases were reported from 23 countries, and 758 cholera-related deaths were recorded, representing month-on-month declines of 16 percent and 22 percent in cases and deaths respectively compared with July. These figures reflect both the remarkable size of the event and the uneven geographic distribution of burden that complicates international and national response planning.
The upsurge’s sustained duration since 2021 has been driven by a mix of factors that converge to increase population vulnerability and transmission risk. Protracted humanitarian crises, conflict-related displacement, seasonal flooding, and disruptions to water and sanitation services create conditions conducive to cholera spread. In many affected areas surveillance systems remain weak, leading to delays in detection and reporting; in parallel, health services are often overwhelmed or under-resourced, limiting timely case management and community outreach. The aggregated data through August 2025 make clear that the outbreak is not a single-country emergency but a multi-jurisdictional event that requires coordinated cross-border action and flexible allocation of limited global resources.
Oral cholera vaccine (OCV) remains a critical tool for outbreak control and prevention, yet the global emergency stockpile has been strained. At the end of August the average OCV stockpile stood at approximately 2.6 million doses, well below the emergency target of five million, constraining the ability to mount large-scale reactive campaigns where needed. Limited vaccine availability forces public health authorities to prioritise high-risk populations and geographic hotspots, which can reduce immediate mortality but leaves many communities unprotected and increases the risk of recurrent transmission in under-vaccinated areas.

Surveillance and data trends from the period illustrate important operational signals. The 16 percent decline in reported cases between July and August 2025 suggests that interventions in some settings may be having a measurable effect, or that seasonal patterns are influencing transmission. However, month-to-month fluctuations must be interpreted with caution because of reporting lags, changing testing and case-definition practices, and variations in health-seeking behaviour among affected populations. Continued investment in timely, high-quality epidemiological surveillance is essential to distinguish true epidemiologic change from artefacts of reporting and to guide allocation of scarce resources such as OCV, medical supplies, and personnel.
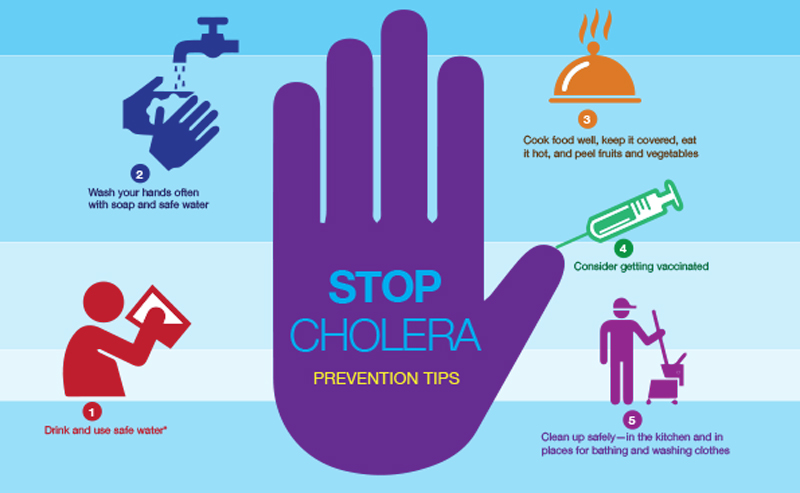
Water, sanitation, and hygiene (WASH) interventions remain the foundation of both short-term response and long-term prevention. Ensuring safe water supplies, restoring or protecting sanitation infrastructure, promoting hygiene behaviours, and coordinating safe burial practices are central to breaking transmission chains. In many affected countries these efforts must be integrated with humanitarian assistance and infrastructure repair after floods or armed conflict. The scale of needs documented in the report points to an urgent requirement for multisectoral collaboration between health, water, shelter, and logistics actors to restore essential services and reduce exposure risks for vulnerable populations.
Clinical management capacity must be bolstered alongside preventive measures. Case fatality rates can be kept very low with prompt rehydration therapy, appropriate use of antibiotics where indicated, and effective referral systems for severe cases. The high cumulative death toll reported through August 2025 highlights gaps in access to care and the consequences of delayed presentation. Strengthening facility readiness, maintaining supply chains for oral rehydration salts, intravenous fluids, and antibiotics, and delivering rapid training and mentorship for front-line clinicians remain priorities in high-burden settings.
The global response also faces strategic resource-allocation dilemmas. With the OCV stockpile diminished and multiple simultaneous outbreaks across regions, international partners must make difficult decisions about where to deploy limited vaccines, technical support, and funding to achieve greatest impact. Investment in surge capacity for rapid reaction teams, mobile treatment units, and surge WASH teams can help reduce mortality while longer-term investments are mobilised. The data through August 2025 make clear that preparedness and resilient systems, not just emergency supplies, determine the difference between localised control and prolonged national or regional outbreaks.
Looking ahead, the report’s aggregated figures call for a two-pronged approach: accelerate short-term lifesaving actions while simultaneously investing in sustainable prevention. Short-term priorities include expanding targeted OCV campaigns where they can be most effective, scaling up WASH emergency repairs, and ensuring uninterrupted clinical supplies and trained personnel for case management. Medium- and long-term priorities must address drivers of vulnerability by rebuilding resilient water and sanitation infrastructure, strengthening routine surveillance and laboratory capacity, reducing conflict- and climate-related displacement risks where possible, and integrating cholera preparedness into broader health system strengthening efforts. The balance of evidence in the situation update through 31 August 2025 suggests that without these combined investments the cycle of outbreaks will continue to impose heavy morbidity and mortality in the most exposed communities.
The multi-country nature of the 2025 upsurge reaffirms that cholera remains a global public health threat tied to inequities in access to safe water and sanitation. To protect lives and reduce future outbreaks, stakeholders at national, regional, and global levels must coordinate strategically and invest both emergency and development resources where they will produce durable reductions in risk. The WHO situation update provides the evidence base for prioritisation and planning as partners work to contain current transmission and build systems that can prevent the next major surge.
Source: Multi-country outbreak of cholera, external situation report #30 -26 September 2025