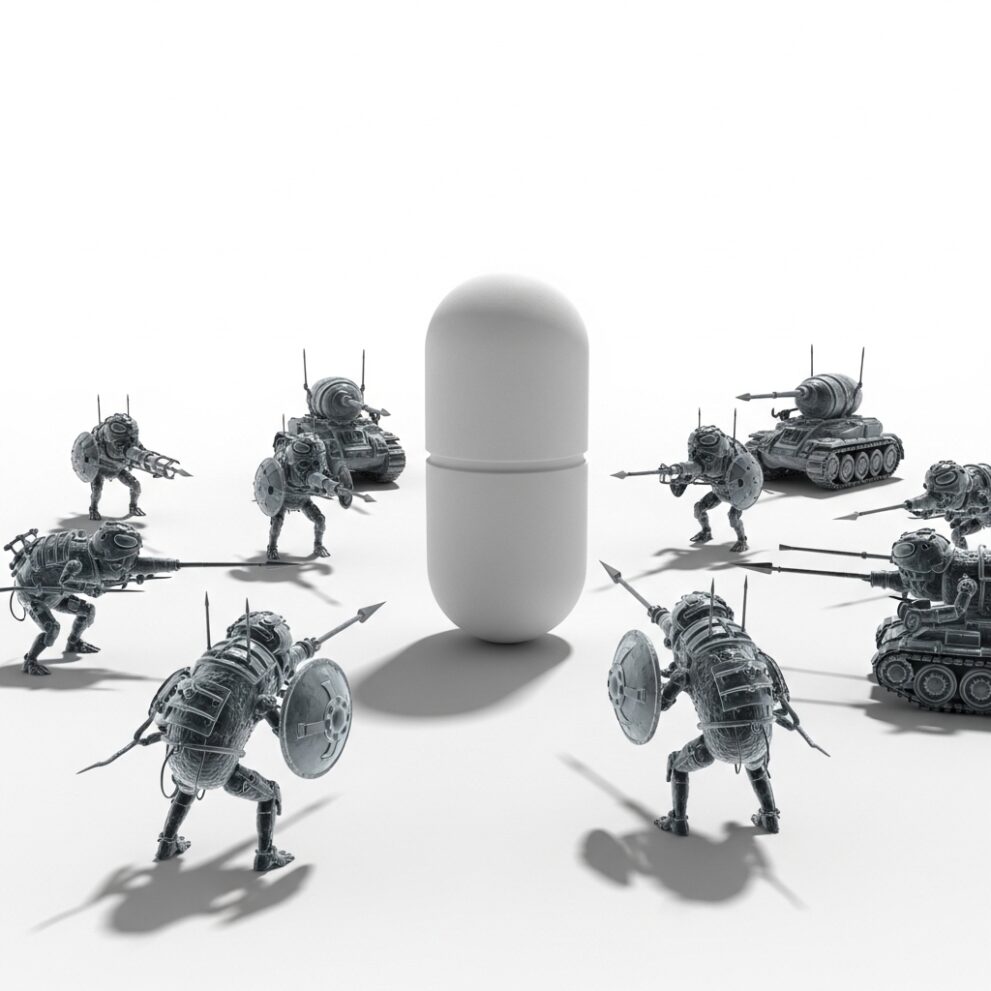
Antimicrobial resistance (AMR) is rapidly becoming one of the greatest threats to global health, and Africa is at the center of this unfolding crisis. The World Health Organization has warned that the misuse and overuse of antibiotics are fueling the rise of resistant microorganisms, creating a scenario where simple infections could once again become fatal.
The statistics are alarming. Currently, one in six bacterial infections worldwide is
“ Imagine a world where a simple infection, such as pneumonia or a poorly healed wound, could be fatal. Does that seem far-fetched? It isn’t. That is the reality that antimicrobial resistance is quietly creating ”
Dr. Filipa Vaz, WHO Laboratory Surveillance Officer
resistant to antibiotics, and in Africa the figure rises to one in five. In 2019 alone, resistant infections caused 1.27 million direct deaths and contributed to nearly five million additional deaths. If urgent action is not taken, projections suggest that by 2050, AMR could claim 10 million lives annually. The economic consequences are equally devastating, with estimates that AMR could cost the world 3.4 trillion dollars per year by 2030 and push 28 million people into poverty. Without effective antibiotics, routine medical procedures such as surgery, cancer treatment, and organ transplants would become extremely risky, threatening decades of progress in modern medicine.
Angola, like many African nations, is not immune to this crisis. Diseases such as tuberculosis, malaria, HIV, and respiratory infections are facing growing resistance, making treatment more complex and costly. The problem extends beyond hospitals and clinics. AMR is also driven by the indiscriminate use of antibiotics in agriculture and food production, as well as the disposal of pharmaceutical waste into soil and water. This creates an environment where resistant microorganisms thrive and spread across borders. As the WHO emphasizes, “Antimicrobial resistance knows no borders. Like COVID 19, it affects everyone, regardless of socioeconomic status or age.”
The response must be integrated and holistic, following the One Health approach, which recognizes the interconnectedness of human, animal, and environmental health. In September 2024, world leaders approved a political declaration at the United Nations with ambitious goals: reducing deaths from AMR by 10 percent by 2030, ensuring global surveillance, promoting rational use of antimicrobials, and expanding access to water, sanitation, and hygiene in all healthcare facilities. Among the commitments are presenting high-quality surveillance data by 2030, ensuring that 80 percent of countries test all bacterial and fungal pathogens, and reducing antimicrobial use in agriculture.

Angola has already taken steps in this direction. During World Antimicrobial Awareness Week, a national workshop was held at the National Health Research Institute, bringing together human health, animal health, agriculture, and environmental sectors to assess the situation and outline strategies. This meeting will serve as the foundation for a National Action Plan against AMR, which will coordinate measures and ensure sustainable responses. Yet, as Dr. Vaz noted, “Antimicrobial resistance is invisible, but its victims are not. Combating AMR requires collective action.”
The role of individuals and communities is critical. Healthcare professionals must prescribe antibiotics only when necessary and follow established protocols. Patients should avoid self-medication, complete prescribed treatments, and never interrupt cycles. Farmers and the food industry must reduce antimicrobial use and adopt safer practices. Civil society and policymakers must support awareness campaigns and enforce regulations that promote responsible use. Every gesture counts, and every decision matters in the fight against AMR.
In conclusion, antimicrobial resistance is not a distant problem but a present and growing threat. It is eroding the effectiveness of life-saving medicines, endangering routine medical procedures, and placing enormous strain on economies and societies. Angola’s efforts to build a national action plan and embrace the One Health approach are commendable, but success will depend on sustained investment, stronger surveillance, and collective responsibility. As the WHO warns, “Without effective antibiotics, we will return to an era where simple infections could be fatal.” The time to act is now, because every delay risks lives, livelihoods, and the future of modern medicine.